Contents
Key Takeaways:
- Advancements in biomaterials and 3D printing are revolutionizing dental bone grafting.
- Stem cell therapies and nanotechnology offer promising avenues for bone regeneration.
- Minimally invasive techniques are enhancing patient comfort and recovery times.
Introduction
Dental bone grafting is a cornerstone of restorative and implant dentistry, enabling the restoration of bone structure to support dental implants, bridges, or dentures. This essential procedure repairs bone loss and provides a stable foundation for various dental restorations, directly influencing the longevity and effectiveness of treatment. The field is transforming rapidly with modern advancements, delivering exceptional outcomes for dentists and patients. Innovations in bone graft for dental implants enhance bone regeneration, reduce discomfort, and speed recovery, signaling a new era of patient-focused care.
New materials and digital technologies are shaping how clinicians approach bone loss, offering tailored solutions that support long-term oral health. With a better understanding of bone biology and innovations in tissue engineering, clinicians now have access to more biocompatible options, minimally invasive approaches, and biological enhancers designed to mimic natural tissue and foster better integration. These advancements mean shorter healing times, fewer complications, and a smoother patient experience. As the science of bone grafting grows, the patient experience and predictability of outcomes continue to improve, paving the way for more widespread adoption and greater confidence in dental implant procedures.
Advancements in Biomaterials
Modern biomaterials are engineered to interact seamlessly with the body, supporting natural bone growth and healing more effectively than traditional solutions. Previously, bone grafting relied heavily on harvesting bone from the patient or a donor, which could result in higher morbidity and increased risk of complications. However, bioactive ceramics, especially those based on calcium phosphates and bioactive glasses, are increasingly used because they promote osteoconduction (bone growth on a surface) and osteoinduction (stimulating new bone). Their unique structures foster a microenvironment that attracts bone-forming cells to the graft site, creating optimal conditions for bone regeneration. Further, these materials can be manufactured in various shapes and porosities to match the defect better, reducing stress on adjacent tissues. Recent research has shown that bioactive glass, for instance, can speed up healing and integration, helping minimize patient healing time and reduce graft failure risk. As new and improved biomaterials are developed, the likelihood of successful graft outcomes and patient satisfaction continues to rise.
3D Printing Technology
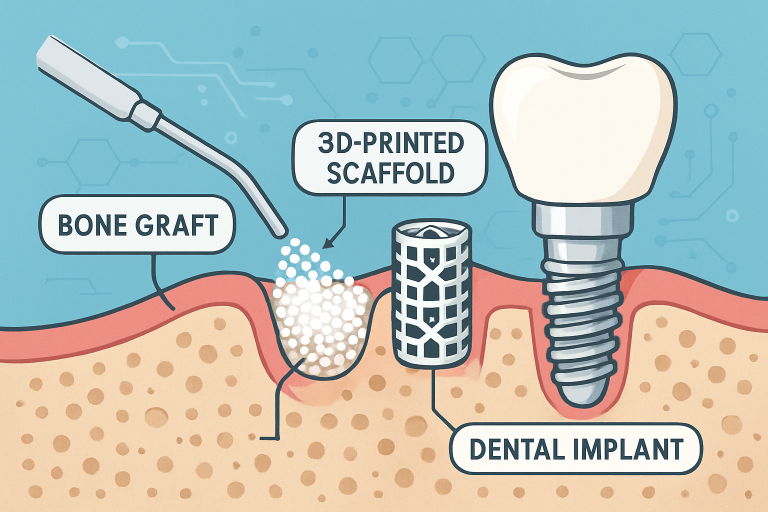
3D printing transforms dental bone grafts’ fabrication, allowing for precise, patient-specific grafts tailored to fit the individual’s anatomy. This next-generation approach simplifies surgical procedures, allowing for more predictable and successful integration. Using digital workflows and patient scans, clinicians can map bone defects in detail and design grafts that fit precisely, eliminating many of the uncertainties of traditional grafts. By customizing the graft’s size, shape, and porosity, clinicians ensure greater contact with existing bone, reducing movement, gaps, and complications post-surgery. Because of these benefits, patients often experience less postoperative discomfort and faster recovery. Using biocompatible printing materials has further expanded the horizons for what is possible with dental bone grafting. In complex cases, 3D printed guides can assist surgeons during placement, enhancing accuracy and reducing surgery time. Ultimately, 3D printing helps accelerate healing and boosts overall restoration success, giving patients restored function and aesthetics faster. For detailed insights, visit this Forbes Tech Council article.
Stem Cell Therapies
Integrating stem cell technology into bone grafting procedures is a promising area of development that may redefine the gold standard in bone regeneration. Stem cells can differentiate into multiple cell types, including osteoblasts (bone-forming cells), thus offering the potential for more complete and rapid bone restoration. The concept typically involves seeding stem cells onto scaffolds, where they can proliferate and regenerate tissue at the defect site, effectively rebuilding bone that closely resembles natural tissue in both form and function. This approach is still under extensive study and rapidly transitioning from experimental to clinical application in advanced practices. Early results indicate that stem cell therapies may significantly reduce healing times, lower the risk of graft rejection, and enable success even in complex or previously failed cases. While regulatory, ethical, and technical challenges remain, stem cell therapies’ potential to improve the predictability and effectiveness of bone grafting is enormous, with the potential to revolutionize traditional bone grafting techniques.
Minimally Invasive Techniques
The current trend in oral surgery is to reduce patient discomfort and foster faster recovery through minimally invasive methods. Recent advances in technique and technology have made it possible to perform bone grafts with smaller incisions, less trauma, and greater precision. Surgeons can minimize trauma to existing tissues using injectable graft materials and miniature surgical tools and expedite healing, reducing the risk of complications such as infection and swelling. These approaches rely on advanced delivery systems that deposit bone-forming materials with pinpoint accuracy, allowing for a more targeted grafting process. In many cases, minimally invasive procedures can be performed under local anesthesia with quick recovery times, making them especially appealing for patients who may be wary of traditional surgery. As these techniques become the standard, patient satisfaction is expected to rise, and the overall success rate of bone grafting procedures is also poised for significant improvement.
Nanotechnology in Bone Grafting
Nanotechnology is ushering in a new frontier by enabling the creation of nanostructured graft materials that more closely imitate the properties of natural bone at a microscopic level. The manipulation of particles at the nanoscale allows these materials to better integrate with the patient’s own tissue, improving their ability to support new bone growth and healing. By engineering grafts at this scale, researchers have enhanced the material’s biochemical and mechanical compatibility, resulting in faster regeneration and more stable outcomes. Early data suggest that nanomaterials spur bone growth and reduce inflammation and rejection responses more effectively than conventional materials. These properties are significant for patients with compromised healing capacities or receiving extensive reconstructions. As research progresses, the hope is that nanotechnology will make bone grafting procedures faster, more reliable, and viable for a broader spectrum of patients, ultimately leading to better clinical outcomes and a broader spectrum of treatment options. For more information, refer to this PubMed article on nanotechnologies in regenerative medicine.
Future Outlook
The future of dental bone grafting lies in the synergy of biology, engineering, and digital technology. As research continues to unlock the secrets behind natural bone regeneration, the field is moving toward truly personalized treatment plans that address each patient’s unique needs and biology. With increased adoption of digital planning, real-time 3D imaging, and regenerative medicine tools, bone grafting procedures are becoming more predictable, accessible, and reliable across a broader patient spectrum. Moreover, global efforts in collaborative research are accelerating these advancements, closing the gap between laboratory discovery and clinical application. Patients can look forward to shorter treatment times, less invasive surgeries, and greater confidence in the long-term success of their dental restorations. It is an exciting time for clinicians and those needing dental implants or reconstructive procedures, as technological and biological frontiers continue to expand.
Conclusion
Dental bone grafting is being transformed by breakthroughs in biomaterials, 3D printing, stem cell therapies, minimally invasive techniques, and nanotechnology. Today’s innovations promise stronger, more predictable outcomes, and a dramatically improved patient experience. With ongoing research and cross-disciplinary collaboration among clinicians, engineers, and researchers, progress promises to remain swift. As science advances, these changes will help clinicians deliver care that supports quality of life and long-term oral health for patients worldwide.