Contents
Key Takeaways:
- Proper preparation of infant formula is crucial to protect infants from potential contaminants and ensure their well-being.
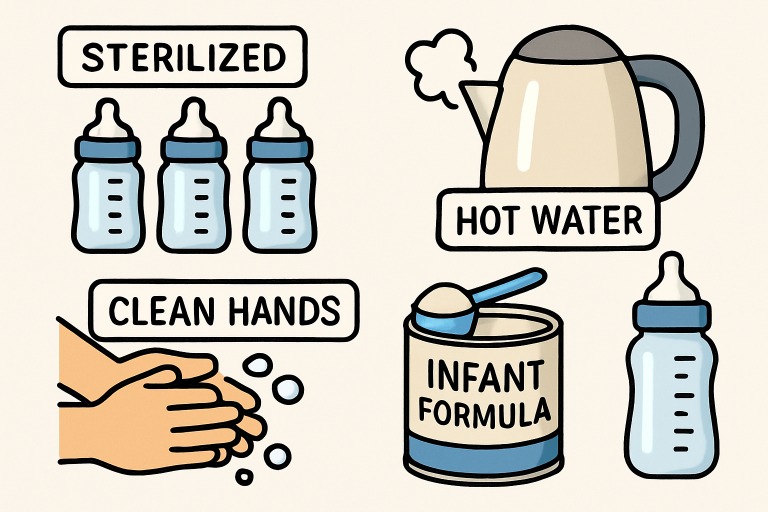
- Heated water, sterilized equipment, and strict adherence to hygiene protocols play pivotal roles in ensuring formula safety.
- Following clear, step-by-step guidelines minimizes the risk of infection and guarantees proper nutrition.
- Emerging research and regulatory updates underscore the ongoing importance of vigilance in the preparation of formula.
Understanding the Importance of Safe Formula Preparation
Ensuring that infant formula is prepared safely is a critical aspect of caring for infants who rely on formula for nutrition. Infants are particularly vulnerable to infections caused by pathogens such as Cronobacter and Salmonella, which can contaminate formula through improper handling or storage. Even small lapses in cleanliness can introduce these harmful bacteria, leading to serious illness in infants.
Parents and caregivers are strongly encouraged to familiarize themselves with best practices for formula preparation to provide optimal nutrition while protecting infants from preventable health threats. Incorporating thorough handwashing, proper sterilization of feeding equipment, and correct handling of both powder and water can significantly reduce the risk. Extensive resources and training are available to guide caregivers and professionals in appropriate practices, such as the comprehensive training offered through the Infant Formula Tech Training program at MSU Denver, which equips them with the knowledge needed for safe formula handling.
Organizations like the Centers for Disease Control and Prevention (CDC) have issued clear recommendations on the preparation and storage of infant formula, emphasizing that all steps from washing hands to measuring formula are essential for infant safety. CDC: Infant Formula Preparation and Storage.
One key element often overlooked is the temperature of the water used in formula preparation. According to public health guidelines, water should be heated to at least 158°F (70°C) before mixing with powdered formula, as this temperature is necessary to kill potentially harmful bacteria present in the powder. Caregivers should allow the water to cool slightly before combining it with the formula to prevent burns. Always shake the bottle to ensure even mixing.
Step-by-Step Guide to Preparing Infant Formula Safely
- Wash Your Hands: Start with thorough hand washing using soap and running water. Dry your hands with a clean towel or allow them to air-dry to prevent the introduction of germs.
- Clean and Sterilize Equipment: Carefully wash and sterilize all bottles, nipples, rings, and preparation surfaces to ensure cleanliness and prevent contamination. While dishwashers with hot water cycles can sanitize, boiling or steam sterilizers are also effective methods for bottles and feeding parts.
- Use Safe Water: Only use water heated to at least 158°F (70°C) to mix with powdered formula. After boiling, allow the water to cool slightly, but mix while it is still above 158°F to ensure safety. For ready-to-feed or liquid concentrates, follow the manufacturer’s guidelines precisely.
- Measure Accurately: Adhere strictly to the manufacturer’s instructions regarding the amount of powder and water. Improper ratios can lead to either undernutrition or dangerous dilution, which can impact infant health and development.
- Cool and Test Temperature: Once mixed, cool the prepared formula by running the bottle under cold water or placing it in a bowl of ice water. Always test the formula’s temperature on the inside of your wrist; it should feel lukewarm, not hot.
Recent Studies Highlighting Safety Concerns
New research consistently highlights the importance of rigorous formula preparation. A pivotal study conducted by Swansea University reported that the vast majority of infant formula preparation machines tested approximately 85% failed to heat water to the recommended 70°C. This shortfall potentially leaves infants exposed to dangerous bacteria, as lower temperatures are insufficient for killing contaminants like Cronobacter. The findings emphasize the importance of caregivers double-checking water temperature, particularly when relying on automated machines or time-saving equipment.
Regulatory Actions and Recommendations
Addressing ongoing safety concerns, regulatory bodies such as the U.S. Food and Drug Administration (FDA) have taken a proactive stance. The FDA has issued warning letters to major infant formula manufacturers in cases of product safety and quality violations. These regulatory actions are designed to protect public health and reinforce industry accountability, prompting stricter monitoring and adherence to manufacturing standards. The FDA’s ongoing oversight ensures that formula products meet the highest safety benchmarks before reaching families.
Common Mistakes to Avoid
- Using Homemade Formula: The FDA strongly discourages the use of homemade formulas. These lack standardized nutritional content and pose significant risks of contamination or nutrient deficiency, which can jeopardize infant health.
- Improper Storage: After preparation, the formula should be used within two hours or promptly refrigerated and consumed within 24 hours. Leaving the formula out longer increases the risk of harmful bacterial growth.
- Reheating Formula: Never reheat previously prepared formula. Reheating can promote bacterial growth and compromise the essential nutrients that infants require for healthy development.
Conclusion
Consistent and careful adherence to safe practices in formula preparation is a non-negotiable aspect of infant care. By following evidence-based guidelines, using the correct water temperatures, and ensuring strict hygiene, caregivers can confidently provide safe, nutritious formula every time. Staying informed through reputable channels, embracing recent research, and monitoring regulatory developments amplifies the safety net for every infant who relies on formula feeding.